- POTS and Salt: What the Science Actually Says - 18 February 2026
- Why the Beighton Score Matters More Than It Should - 18 February 2026
- Brain Fog in EDS, POTS and Long COVID: Causes and Practical Ways to Cope - 13 February 2026
If you live with Postural Orthostatic Tachycardia Syndrome then you already know that standing up is not always as easy as it sounds. POTS is a form of dysautonomia where the heart rate will increase abnormally on standing, often brings with it dizziness, palpitations, fatigue and that all too familiar brain fog along with it (1). For some people it is like the floor drops away. For others it is more subtle but relentless: a constant battle against gravity.
POTS does not exist in isolation either. It often cooccurs with joint hypermobility and Ehlers Danlos syndromes as the laxity of the connective tissues means more blood is able to pool in the lower body exacerbating autonomic symptoms.(2) If you are hypermobile, this combination can be a perfect storm. Lax veins, shaky joints, gastric problems, fatigue. It all layers up a bit, like a cake of crappy symptoms.
One of the first things many people who have clients with POTS, will recommend with respect to managing POTS is increasing salt and fluids. The logic is pretty simple and it’s based on the physiology. Sodium makes the body retain water. What this means is that more sodium equals more circulating volume. More circulating volume can translate into lower dramatically heart rate spikes when you are standing (3). On paper, it makes sense.
But then the questions start.
How much salt is enough? How much is too much? Should You Use Table Salt, Capsules or Electrolyte Drinks? What about long term risks to your heart and kidneys? And if you are hypermobile, and have, let’s say, an upset of the gut as well, or you get nausea, or you get bloat, how realistic are you that you are drinking three litres a day?
These are the conversation that get’s skipped out over.
In this article, I am going to walk you through what the science actually says on this topic of salt and electrolytes in POTS. We will examine how these recommendations have been made, what the clinical trials reveal about them and how to put this advice into practise in real life. Especially if you are dealing with hypermobility or EDS on top of POTS
The aim here is simple. Evidence based. Brand neutral. Practical. So that when you sit down with your healthcare team you are not guessing. You know the reasoning, the dangers and the trade offs.
This article covers:
ToggleHypovolemia, venous pooling, and autonomic regulation
When we discuss POTS and salt, we are actually discussing blood volume and how your body deals with gravity.
Multiple studies are suggestive that a sizable subset of individuals with POTS will have decreased plasma volume and total blood volume compared to the healthiest controls.(3,4). In more basic terms, there is less fluid in the system. That matters.
When the blood volume is low, the body compensates. One of the chief ways it does this is by boosting levels of hormones such as norepinephrine when you get up (3). Norepinephrine is the sympathetic system response. It constricts the blood vessels and propels the heart to pump faster. That is great in the short term, but in POTS these can soar out of control, causing tachycardia and many of the symptoms you are experiencing.
Now add in the venous pooling.
If blood accumulates excessively in the lower body, be it because of lax connective tissue, the inability of veins to respond adequately to changes in body position, or impaired autonomic control, then the effective volume passing to the heart falls even lower (2,3). Less blood reaches the heart. Less blood is circulated to the brain. The body responds by raising the heartrate even further. That is orthostatic intolerance at work.
This is why salt and water are on centre stage in POTS management.
Sodium is the predominant extracellular cation, and it plays a major role in determining the osmolality of the plasma. In layman’s terms, sodium helps to retain water in the blood. Where sodium goes, water follows Increases in sodium intake results in increases in the extracellular fluid and plasma volume, at least on the short to medium term (3,4). That increased volume allows less of a drop in the central blood volume as you stand up and blunt the heart rate increase.
It does not cure POTS. But from a physiological point of view, it makes sense.
Key electrolytes for POTS: sodium, potassium, magnesium, calcium, chloride
When people hear the word electrolytes it seems to be technical sounding or frightening. In fact, electrolytes are nothing but charged minerals which are dissolved into your bodily fluids. They help nerves to send messages, muscles to move and fluids to be moved from one compartment to another in the body. Without them nothing goes smoothly.
Each of the electrolytes has a slightly different job. And when you live with POTS, that’s a difference you need to know.
Sodium (Na+) is the major positive ion outside of your cells. It has a dominant role in regulation of plasma osmolality, blood volume and blood pressure (3). In POTS the sodium thought to be the cause of the problem is the key focus due to its direct effect on the circulation. Increase the sodium and you increase the body’s ability to retain water. That increased volume can lessen the increase in the rate of the heart beat that occurs as you stand up.
Potassium (K+) is the primary positive ion in the interior of your cells. It is necessary for the maintenance of the electrical potential in the cells, particularly the heart and skeletal muscles. In simple words, it helps your heart to beat properly and your muscles in their normal functioning. Potassium also cancels out some of the effects of sodium on blood pressure. (5, 6) That sodium to potassium ratio becomes an especially important factor when we consider longterm cardiovascular health and if, especially, someone is on a higher sodium plan.
Chloride (Cl-) is typically a companion of sodium in dietary salt. It helps people maintain a balance of fluid, and is involved with acid base regulation. While hardly a star in the system, it is part of the same system.
Magnesium (Mg2+) and calcium (Ca2+) play an important part in the operation of the muscles, nerves, and blood vessel tone. If levels are off, you may experience muscle cramps, fatigue, irregular heartbeats or the way blood vessels behave. Many individual littera affected by hypermobility speak of muscle tension or cramping, so I would not say that these minerals are irrelevant to the bigger picture.
For POTS we are predominantly pulling the sodium control of the hormone because of its clear impact on blood volume and sympathetic function. But that is not to say that the other electrolytes are not important. Potassium, magnesium and calcium are involved in shaping the stability of the cardiovascular system and may determine how a person tolerates a higher intake of sodium (3, 5).
If we want to simplify things, then caricaturize sodium as a broader umbrella and the problem can be dealt with, but then we run the risk of caressing a problem that is anything but simple.
Evidence for high salt intake in POTS
Clinical trials of high sodium diets in POTS
For years, high recommendations employed for salt in POTS have been based on more physiology and clinical experience than good controlled trials. The theory made sense. This was supported by the lived experience of clinicians and patients. But robust data were limited.
That all changed with a landmark crossover study by Raj et al in 2021 (3).
In this trial, 14 women with POTS participated in two phases or six day diet. One phase was a very low sodium intake, around 10meq per day. The other was a very high sodium intake, around 300 mEq per day, some 6.9 grams of sodium, or 17 grams of salt. The order was randomised. Thirteen healthy women were considered as control (3).
The results were important.
On the high sodium diet, subjects with POTS exhibited:
Increased plasma and total blood volume (3).
Plasma norepinephrine reduced levels of (3)
Reduced upright heart rate and reduced increase in heart rate from a supine to erect position although many still had diagnostic criteria fulfilling POTS (3).
This is important as it is directly related to the physiological model. Increasing sodium increased the volume of blood. Expanded blood volume lowered the sympathetic activation. Suppression of the sympathetic limited the tachycardia.
In other words, salt did what the theory predicted it would do.
However, he goes on to say, “We must not be caught up in the clouds.” The study was short. Only six days per diet phase. The sample size was small. And it lacked an assessment of long term cardiovascular outcomes (3,7). We can’t assume that improvements over the short term automatically translate into improvements over the long term with regard to safety.
Beyond this study, there is research into oral rehydration solutions in children with POTS that suggests sodium containing solutions are able to improve how children and selected patients tolerate orthostatic changes and their symptoms. (8, 9) Some recent work has even attempted to determine which children may be most likely to respond using some such markers as blood counts and blood pressure parameters (8, 9). This is a step towards a more individualised approach rather than the one size fits all salt prescription.
What changes: volume, norepinephrine, heart rate
Looking closer at the high sodium arm of the Raj study, a plasma volume deficit observed in POTS observed during low sodium intake was basically eliminated (3). Total blood volume came near to normal in comparison with healthy controls (3). That is not a subtle shift. That is a measurable physiological corrective response.
Standing norepinephrine decreased substantially with this expansion in fluid volume (3). Since norepinephrine is a marker for activation of the sympathic nervous system, this indicates that the body was no longer required to compensate as aggressively when upright.
The response of heart rate was no different. Upright heart rate was reduced, and the increase from supine to standing was reduced (3). Participants also reported improvements in their symptoms although the study was not designed to assess detailed quality of life changes (3).
Taken together, these findings provide quantitative support for what most clinicians already suspected was true. Salt loading is a treatment that can decrease orthostatic tachycardia and can help beat the dizziness and palpitations, especially in hypovolemic forms of POTS (3,4).
It is not a way of normalising everything. But it can have a profound change to the physiology.
Limitations of the evidence and who may not respond
Now we need to add some nuance.
First, these trials were short term, from days to weeks. They do not inform us on what happens after years of sustained high sodium intake in terms of blood pressure, renal function or cardiovascular risk (3,7). That lack of knowledge is important.
Second, subjects in these studies were relatively young and had no major comorbidities. The findings may not be applicable in older people, or people with established hypertension, kidney disease or increased cardiovascular risk (3,7).
Third, not all POTS has hypovolemia as the underlying motivation. In hyper adrenergic or neuropathic variants autonomic dysfunction and vascular abnormalities can be the predominate picture (1,4). In these situations, salt loading may be of limited benefit. For some people, it may even increase, if sympathetic tone is still high, this may make symptoms such as headache or palpitations worse.
So where does that leave us?
Diet high in sodium is physiologically plausible and based on evidence in the short term, controlled data. For many people with POTS (especially for people with demonstrable low blood volume), they may be helpful (3,4). But they are not a cure all. They are a tool. And like any tool, they have to be used carefully and individually tailored to the person sitting in front of you.
Long term safety: balancing POTS benefits with cardiovascular and kidney risk
This is the portion of the salt conversation which often gets swept to the side.
If you’ve got POTS, and salt really does help you to get through the day, then it can feel like a lifeline. But it’s also fair to ask the unpleasant question, what does this mean long term? Especially if you’re taking levels of sodium way too far beyond public health guidance.
What we know about high salt and blood pressure in the general population
In the process, in general population, large epidemiological and interventional study has consistently associated higher sodium intake with higher blood pressure, and higher risk of cardiovascular disease and stroke despite there’s still some debate about the exact dose response curve, and also about what “optimal” intake really looks like (10,11). The general direction of movement is not ambiguous. More sodium tends to push the blood pressure up.
We also know that small decreases in sodium consumption will lower blood pressure in both hypertensive and normotensive subjects, and some cohort studies link increased sodium consumption with increased rates of cardiovascular events and kidney disease (10,11). So if you are somebody who is salt loading for POTS you are going into this area of a place where the population level evidence starts to raise an eyebrow.
One detail that seems to get overlooked is that it is about these parts sodium. The Trials of Hypertension Prevention follow up study utilised repeated 24 hour urine collections and showed that a higher urinary sodium to potassium ratio was linked to a very significant increased risk of subsequent cardiovascular disease (6). That leads to a theory the balance between sodium and potassium is important and not just the number of sodium in the headlines.
So even in a POTS context, it is worthwhile thinking not only have “more salt equals bettered” but might think about the broader, more general diet pattern in conjunction with it.
Kidney health and sodium
It is in the kidneys that the long term salt conversation gets even more serious.
Chronic high sodium consumption is linked to glomerular hyperfiltration and is a potential cause of faster kidney damage in susceptible populations (12,13). You do not have to have diagnosed kidney disease for this to be of relevance. It comes into play when another person has risk factors, such as hypertension and diabetes, or family history of kidney problems.
Systematic reviews in people with diabetes demonstrate a reduction in blood pressure with reduced sodium intake and may reduce the barriers in diabetic kidney disease progression, although the results have been mixed and low to moderate quality (14) That nuance matters. This is not a clean, tidy story. But the general direction is still the same. In vulnerable individuals, high sodium will set the system in the wrong direction.
This is where individual context becomes all things.
For the younger individual with normal BP and kidney function, a close following high sodium diet may make sense if the benefit to POTS was significant and other options were limited. But in the case of someone who has established hypertension, diabetic kidney disease or a strong family history of stroke, the cost and benefits of aggressive salt loading may be more complex and the limits and monitoring requirements may be more stringent (10,11,14)
It is not about fear. It is about risk management..
How to individualise salt targets with your medical team
This is why it is necessary to personalise POTS salt recommendations.
Most public health advice is targeted on reducing the number of sodium consumed, POTS guidance is often in the range of 3,000 to 10,000 mg of sodium per day. (1, 15) Those numbers all look completely contradictory on paper, but they are aimed at different problems. Still, they should not be blindly applied.
Expert centres such as the Cleveland Clinic advice that patients with POTS, with the assistance of their clinicians, can have a goal of perhaps about 3,000 to 10,000 mg per day of sodium, with the amount within this range needing to be adjusted based on the individual’s symptoms and problems from other health conditions (15). The most important phrase there is depending on symptoms and comorbidities. In other words your body, your risk factors your response.
A practical approach typically appears as follows:
Start with a baseline check blood pressure, kidney function (creatinine, eGFR) and broader cardiovarskors Risk Factors (7).
Increase gradually toward the intermediate and low end and only by titration move upward if necessary for symptoms control (4,7).
Recheck periodically, using blood pressure and kidney function at home as well as at the clinic and also, if applicable, urine albumin or protein especially if you are on higher doses for months or years.(7, 14)
Done properly, this becomes a measured trial as opposed to a forever decision. It provides you room to be able to discover lowest effective dose that allows improvement in symptoms, however not casually sliding into an array that could soon be problematic later.
Is salt or electrolytes better for POTS?
This is one of the same popular questions I get.
Do you just add some salt to your food and drink more water? Or do you need a specific formula of electrolytes? Powders and tablets and sachets and the lot
The honest answer is that for the majority of people with POTS sodium is the key driver. But the context matters.
Salt alone vs full electrolyte solutions: mechanisms and evidence
From a physiological point of view, anything that increases sodium and water at the same time should increase plasma volume in hypovolemic POTS (3,4). That sodium could be from the table salt, salty food, salt capsules or an electrolyte drink. The body is not much concerned with the branding. This is concerned about sodium and fluid.
In clinical practise, both approaches are applied. Some people are just salt and water people. Others use solution that is balanced with electrolytes that contain both sodium and potassium; sometimes also magnesium and glucose (4,8).
When we are reviewing the research, the strongest evidence is around sodium itself. Randomised trials in POTS have manipulated sodium intake only, rather than any other electrolytes (3). An increased sodium intake leads to an increased plasma volume and a decreased orthostatic tachycardia. That part is supported.
What we do not have good evidence for is that the addition of extra potassium or magnesium, above meeting normal daily requirements, directly improves for POTS outcomes (3,4). That does not mean that they are not relevant. It just means the sodium is the principal lever of therapy that is so far studied.
So in pure evidence terms, it is sodium load that is the central mechanism.
When plain salt plus water may be enough
For some people, especially those who tolerate salty food well, plain salt plus adequate water is entirely sufficient.
If you can reach around 3,000 to 10,000 mg of sodium per day using food and measured salt, and you are consistently drinking 2 to 3 litres of fluid daily, you may not need anything more complicated (1,15). PoTS UK suggests that many adults may require an additional 6 to 10 grams of salt per day, which is roughly 2.4 to 4 grams of sodium, on top of usual dietary intake, though targets should always be individualised (1).
This approach has advantages. It is simple. It is usually cheaper. It avoids flavourings, sweeteners, and additives that some people do not tolerate well. And for those without significant gastrointestinal issues, it can fit naturally into regular meals.
For many people, that is enough to meaningfully improve symptoms (1,4).
When balanced electrolyte solutions are preferable
There are cases where electrolyte solutions are more sensible choices.
If you are losing fluid by having diarrhoea, vomiting or heavy sweating you are not just losing sodium. You are also losing potassium and other electrolytes. (8) In that context a balanced solution can help to bring back what has been lost.
If you have trouble with chronic nausea, early feeling full or gastroparesis, which is very common with hypermobility and POTS, eating meals high in salt may not be realistic. Sipping fluids throughout the day may be easier than eating copious amounts of salty foods (2,8).
In the case of acute dehydration, such as a viral infection, oral rehydration solutions are very helpful. A combination of sodium and glucose promotes water absorption in the gut through a phenomenon known as sodium glucose cotransport (8,9). This is the reason, World Health Organisation style oral rehydration solutions contain specific ratios of sodium and glucose. They are formulated to optimise absorption in the case of diarrhoeal illness (8).
For everyday purpose POTS management, most people do not require full strength medical ORS. Many consume formulations of lower glucose electrolytes that supply some 500 to 1,000 mg of sodium per serving, varying the number of servings according to daily sodium needs (4,8).
So it’s not really salt vs. electrolytes. It is what your body requires in your particular situation.
If your primary problem is low blood volume and your tolerance for food is good, salt and water may be all that is necessary. If you are experiencing fluid losses, poor oral intake or are suffering an acute illness then a balanced electrolyte solution might be the smarter choice.
Which electrolytes are important for POTS?
When people begin increasing salt for POTS, the discussion all too often goes salt sodium crazy. And that makes sense. Na is the primary therapeutic leverage. But it is not the only electrolyte which matters.
If you are changing one component of a finely balanced system, you must know how the rest of that system will react.
Sodium: the main driver of blood volume
The most important role of sodium in POTS management is to boost the extracellular fluid volume and support the blood pressure and cerebral perfusion when you stand (3). If low effective circulating volume is your physiology, sodium is of central importance.
The high sodium trial which we spoke about earlier found that the addition of sodium greatly increased plasma volume and decreased orthostatic tachycardia for a group of people with POTS (3). That is not theoretical. It is measurable. Clinical recommendations of about 3,000 to 10,000 milligrams (mg) of sodium per day are aimed at producing this volumetric effect. (1,3,15) The upper limit of that range is usually reserved for more severe symptoms and patients who have no significant cardiovascular risk.
It is also important to be clear of terminology.
Salt and sodium are not either one. Salt is the common name for sodium chloride. Sodium is but one component of that molecule. Salt is about 40 percent weight sodium. So 10 grams of salt would give us 4 grams or 4,000 mg of sodium (1,15). If you are watching intake, this is a big difference.
Sodium is the main driver. But it is not an island in the sea.
Potassium: counterbalance, heart rhythm, and sodium to potassium ratio
Potassium plays the different, but equally important, role. It is critical for heart rhythm, muscle contraction and regulation of blood pressure (5,6). Whereas sodium can cause an increase in blood pressure, potassium can help counteract some of the effects.
Increased consumption of potassium is linked to reduction in blood pressure especially in hypertensive individuals. Meta analyses find that there is a dose dependent decrease in blood pressure with potassium supplementation.(5) That goes really far when the person with POTS is actually trying to increase sodium intake.
Longterm studies data have indicated that urinary sodium to potassium ratio is a better predictor of cardiovascular disease than sodium or potassium alone (6). In the simplest way, it is not only how much sodium you eat. It is all about the balance between sodium and potassium.
For someone following a higher sodium eating plan for POTS to ensure adequate levels of potassium through food may aid in protecting long term cardiovascular health, assuming there is normal kidney functioning and medications allow this (5,6). Some practical sources are fruits, vegetables, legumes, or dairy.
What is not supported is high dose potassium supplementation for all. Excess potassium can cause danger, especially for those with kidney impairment or for those who take ACE or ARB inhibitors as well as potassium sparing diuretics (5). Heart rhythm disturbances is not a problem to experiment with. This is one area where clinician oversight is really important.
Magnesium and calcium: muscles, nerves, arrhythmias, and cramps
Magnesium and calcium have an effect on neuromuscular excitability and vascular tone. Population studies have found an association between low intakes of magnesium and increase of blood pressure and cardiovascular risk. Adequate calcium intake will promote a healthy bone, and modestly affect blood pressure especially when an individual has a high sodium intake (10).
In the case of POTS specifically, magnesium may be resorted to empirically for muscle cramps, migraine or palpitations. But good randomised trials in POTS are lacking (2). So while it might be beneficial to some to some of the symptoms, it is not an integral, evidence based POTS therapy the way that sodium is.
From a safety perspective, achieving recommended intakes through the diet is absolutely in most cases easy and safe. Nuts, seeds, whole grains, leafy green vegetables, dairy products or fortified products will cover the majority. Higher dose supplements should be used with expertise, particularly where there is kidney disease and problems with excreting magnesium and calcium may be experienced (14).
Chloride and bicarbonate: acid base balance and ORS formulas
Chloride is normally found alongside sodium in most salts. Its major function is maintaining the electro neutrality and contributes to acid base balance. In day to day POTS management, the chloride intake is usually the same as the sodium intake and does not usually require separate consideration.
In oral rehydration solutions, the sodium chloride is usually mixed with citrate or bicarbonate. These components help to correct acidosis in diarrhoeal illness, as well as help to correct fluid absorption (8). It’s just the same physiological principles if you are using oral rehydration solutions in a period of acute dehydration in POTS.
For management from day to day, however, chloride will not typically need to be manipulated in any targeted way. If you are working on increasing sodium through salt or electrolyte solutions then chloride is almost always going to follow.
Overall, sodium is the cornerstone to electrolyte management in POTS. But long term safety and cardiovascular safety is reliant on the bigger balance. Potassium, magnesium, calcium and even chloride take supporting roles. The aim is not necessarily more of the same sodium. It is the lowest dose of sodium required in a diet well balanced for other components.
How much salt should a person with POTS have per day?
Adult targets and scientific basis
Most specialist centres and patient charities suggest a minimum daily intake of about 3000 to 10000 mg of sodium per day (this need must be under medical control), for adults with POTS. That is much higher than general public health advice, and is specifically to increase blood volume (1,3,15).
That range is not random. It is derived from a number of sources.
First, experimental high sodium diets, including 300 mEq of sodium per day, which is approximately 6.9 grams of sodium, have been shown to have a centered effect on increasing plasma volume and lowering orthostatic tachycardia (3). And that gives us an anchor point here physiologically.
Second, from our clinical experience, some patients, especially those with overt hypovolemia or with physical needs that are higher than average, require intakes at the higher end of that range in order to feel like they are receiving meaningful relief from symptoms.1,3 Others respond well to markedly less.
Third, safety matters. Extreme intake of sodium is not suitable for everyone. Older people and individuals who are at a higher cardiovascular risk may require more conservative targets (7,10).
PoTS UK recommends that some adults may have to take an extra 6 to 10 grams of salt per day, which amounts to 2.4 to 4 grams sodium, in addition to normal dietary intake (1). The most important thing to note is that this is in no way a universal prescription. This is a starting framework that needs to be personalised and monitored.
More in, this is Not Necessarily Better. The goal is the lowest effective dose which improves the symptoms.
Younger people, older adults, pregnancy, and comorbidities
Salt recommendations cannot be copied and pasted across age groups and life stages.
Children and adolescents
In children with POTS, the evidence base is small. There is no universally agreed safe upper limit and excessive salt consumption may lead to a higher risk of high blood pressure or a strain on the kidney (1). Paediatric salt strategies should thus be led by clinicians that are experienced in paediatric cardiology or autonomic disorders, with careful monitoring (1,8).
Nonpharmacological measures, such as increased consumption of fluids, salt, compression and exercise, are sometimes first line measures and often adequate in teenagers (1,16). Some paediatric protocols use dosing in the region of 2 mmol of sodium per kilogram per day in divided doses or use slow sodium preparations. But this has to be individualised and supervised (16).
Pregnancy
Pregnancy layer upon layer.
Blood volume will naturally increase during pregnancy and both POTS symptoms and hypertension risk may change. Salt recommendations need to consider maternal blood pressure, kidney function and foetal growth (17).
Reassuringly, the incidence of POTS alone does not seem worse than the general population regarding miscarriage, stillbirth or preterm birth rates (17) Symptom flares are frequent for the first trimester, overlapping sometimes with hyperemesis gravidarum (17). Conservative measures, including trying to drink about 3 litres of fluid a day, 6 to 10 grammes of salt, if there is no hypertension or preeclampsia, compression garments and left lateral rest, are the usual ones (17). Close cooperation between obstetric and cardiological forces is imperative.
Older adults and comorbidities
Older patients, as well as patients with diabetes, chronic kidney disease, and known hypertension, often need more conservative sodium credit limits and closer monitoring (10,11,14). In these groups, the risks over the long term with respect to cardiovascular and renal may outweigh the rewards of having an extremely high sodium intake.
Practical ways to count sodium
It is one thing to know your target. Translating that and having to apply that to everyday life is another.
A few common sense strategies make a difference:
- Read labels carefully. In many countries, downsodium is listed on per 100 grams and also on serving. If the label uses the word salt instead, multiply by 0.4 to obtain an estimated value for sodium.(1)
- Track your baseline intake for several days using a nutrition app or an organised worksheet to get an idea of where you are starting from (4). Most people underestimate what they are eating.
- Gradual increase in dose (in steps of approximately 1,000 to 2,000 mg sodium per day) should be maintained, subjects should be monitored for symptoms, BP and weight (4,7). Sudden weight gain or swelling grounds that you could be overloaded with fluids.
This process should have a sense of being measured so as not to be in rush. You are not trying to win a competition for the highest amount of salt intake. You are trying to stabilise your physiology and are protecting your health in the long term.
What kind of salt should I use for POTS
This is where the internet can be noisy.
Pink salt. Sea salt. Rock salt. Celtic salt. Iodised salt. Unrefined. Mineral rich. “Natural.”
When you are trying and getting about POTS symptoms, it is easy to wonder whether the type of salt makes a difference.
Coming from a physiological point of view, the answer is not as difficult as marketing leads us to believe.
Table salt vs. “natural” salts
If we’re strictly going by the amount of sodium however, culinary salts are quite similar. Refined table salt, sea salt and rock salts such as Himalayan salt are all mostly sodium chloride. The differences are small and are often related to the trace minerals or processing methods.(18)
Grams for grams, their capacity of increasing sodium uptake and increasing blood volume is basically the same (18) It is your body that reacts to the sodium, and not to the colour of the crystals.
For POTS management, the decision may come down to many practical considerations:
Taste preference
Cost and availability
Additives, e.g. iodine, anti caking agents
There are those who prefer minimally processed sea or rock salts because they desire to avoid additives. Others may benefit from iodised table salt if the intake of iodine is a concern (18). From the point of view of symptoms of POTS there seems to be no conclusive proof that one type of salt helps produce a better response to orthostasis than another.
It is the sodium content that is important.
Trace minerals: meaningful or marketing?
Many “natural” salts are sold as superior based on the fact they contain some trace amounts of magnesium, calcium or other minerals.
In reality, the amounts of these minerals, which are contained in salt, are very small compared with recommended daily intakes (18). Even if you are taking greater amounts of salt for POTS, the amount of these trace minerals in overall nutritional status is negligible.
If you are seeking magnesium or calcium it is a much better idea to get it from food or specifically supplementation than from small amounts in special salts (10,18).
This is not to discard preference. If you like the flavour of a certain salt and you’re able to consistently hit your sodium goal by using that salt, well, that’s important. But, from the standpoint of clinical medicine, trace mineral claims are more marketing than meaningful intervention.
Iodine and public health considerations
It is where things get more important with the salt conversation to using iodine.
In areas of iodine deficiency, iodised salt is an important means of prevention of goitre and thyroid dysfunction (18). If you are dramatically raising the amount of salt intake for POTS, it is worthwhile to consider where your iodine is coming from?
If you use simply non iodised salts as well as little fish, dairy or eggs, you may not get a lot of iodine. On the other hand, if you eat large amounts of iodised salt as well as plenty of other iodine rich food, intake could be excessive. Too little can affect the thyroid function both deficiency and excess are possible.
For this reason, it is rational to talk to your clinician about iodine status with your clinician should you be making major changes to salt intake (18). Especially if you have thyroid symptoms and or a history of thyroid disease
At the end of the day the best salt for POTS is the one that is proven to provide sodium reliably, in a manner that you are well tolerated, according to your diet, and that matches your overall health picture.
Oral rehydration solutions vs daily electrolytes
When people hear “electrolytes” they often lump it all together. But there is a significant difference between medical oral rehydration solutions and the products offered every day for products marketed for sport or for chronic conditions.
They are not the same thing. And they are not created for the same purpose.
WHO style ORS: when and why to use it
World Health Organisation oral rehydration solutions were developed for treating dehydration due to diarrhoeal illness. Their formulation is conscious. They are of specific concentrations of sodium, usually about 75 mEq per litre, glucose and other electrolytes (8). The glucose is not there for the flavour. This helps to absorb sodium via the small intestine, sodium glucose cotransport mechanism (8). Where there is sodium, there is going to be water with it.
In the setting of acute fluid loss, such as gastroenteritis, high output diarrhoea or repeated vomiting, ORS can be extremely successful at preventing or correcting dehydration (8). For a person with POTS, where you already have a very fragile variable, blood volume, in the case of acute dehydration can dramatically exacerbate your symptoms. In those times, a well formulated ORS can be very helpful.
There is also work in the clinic with children with POTS that describe the use of ORS as a treatment strategy. Some research indicates that selected children have enhanced orthostatic tolerance using ORS and researchers are now attempting to find out which patients will be most likely to respond (8,9). This drives home the notion that the mode of delivery of sodium and the context of the delivery are important.
But ORS did not develop as a day to day lifestyle drink.
Daily maintenance electrolytes for POTS
For purposes of everyday POTS management in most people don’t require full Strength ORS. Many people consider it too salty or too sweet and may not offer more glucose than is needed for routine use (4,8).
Maintenance electrolyte products, usually products marketed for athletes or individuals with orthostatic intolerance, are often milder than these. They commonly contain:
- A serving of sodium should be about 500 to 1,000 milligrams (4).
- Smaller quantities of potassium and occasionally of magnesium (4).
- Flavourings and sweeteners and acids including citric acid for taste (4).
These could help to make it easier to meet daily goals of sodium intake, especially for individuals who have a hard time with heavily salted food options or who require options that can be easily carried around (4). But formulations differ greatly. Some products are close to medical ORS composition. Others are basically flavoured water with some sodium.
Reading the label matters. The key number to look at is not marketing but sodium per serving.(1,4)
Sugar free vs glucose containing formulas
Glucose increases the absorption of sodium and water in the gut via the sodium glucose copot mechanism. That is why medical ORS has a calibrated amount of glucose (8). In situations of acute dehydration or poor oral intake, that glucose can actually be for improving rehydration and providing needed energy.
For someone who’s eating well otherwise and taking electrolytes as part of their routine POTS management, there may not be a need for extra glucose. Dietary carbohydrates are already a source of substrate for absorption and energy.(4,8) In these cases, sugar free formulations may be absolutely reasonable.
High sugar sports drinks are another category all together. They are sometimes higher in sugars than necessary to ensure the best sodium absorption and may cause glycaemic instability or gastrointestinal upset (4). For sufferers of POTS who already struggle with postprandial symptoms or reactive hypoglycaemia this can, of course, be counter productive.
The decision on whether to use suga free or glucose containing formulas should be based on your hydration status, overall diet, metabolic health and tolerance. The goal is good absorption of the fluids without causing any new problems in the process.
Popular electrolyte formats and what patients like
Once someone has made a decision to increase sodium, the question becomes a practicable one.
How are you going to get it in to begin with?
There is no one best format. What works can often come down to taste, tolerance, budget and lifestyle.
Powders, tablets, capsules, drops, DIY mixes
Electrolytes for POTS exist in a number of forms, each of which have pros and cons.
Powders are dissolved in water and have a flexible dosing. You can change the concentration depending on how much sodium you need on that day and they come in a wide range of flavours (4). For most people, such flexibility is a benefit.
Effervescent tablets are dissolved in water and are convenient for travel or when you are at work. The trade off is that the amount of sodium provided by each tablet can be rather modest and therefore, to achieve higher daily targets, multiple servings may be required (4).
Capsules, sodium chloride capsules or combination electrolyte capsules, are popular with people who dislike drinks with salt, or require precise dosing (4). They can help make quantification of intake easier. But they need to have good fluid with them as well, otherwise they don’t serve the purpose.
Drops or liquid concentrate may be added to nearly any drink. These are often marketed as containing minimum taste or additives which is attractive for people sensitive to flavourings (4).
Then there are DIY mixtures. Some patients combine table salt, potassium salts and sometimes magnesium salts by published recipes. This is sometimes more cost effective, particularly when taking them over a long period of time. But it requires careful measuring and medical supervision. Overdoing either potassium or magnesium comes with actual risks, especially in case of people with kidney impairment (4,8). This is not something to guess your way through.
Each format delivers sodium. The difference lies in the areas of convenience, tolerance, and control.
Hypermobility patient perspectives: taste, GI tolerance, convenience
For people with hypermobility or EDS, the choice of having this in formats can take an even more important representation.
Nausea, impaired gastric motility, food sensitivities and potential mast cell activation symptoms are not uncommon in this group (2). Strongly flavoured or high coloured electrolyte drinks may be very hard to tolerate. Artificial sweeteners, citric acid and some additives can cause some people to experience symptoms.
In patient communities, capsule formulations and low additive, unflavoured powder are commonly favoured as the formulations offer less patient exposure to flavourings and sweeteners (2). Taste fatigue is also real. Drinking litres of strongly flavoured fluid every day can become tiresome.
There is a variety in the way the gastrointestinal response is. Some people find either slow release of sodium in tablets, but it is better if very concentrated capsules are used to irritate the stomach? Others tolerate small and frequent sips of a more dilute solution much better (2). On the flip side, highly concentrated salty beverages can cause nausea in some people, in which case it is helpful for people to split intake into smaller doses at regular intervals (2,4).
There is no universal rule in this regard. The right format is the one that can be dealt with by your gut on a constant basis.
Cost, availability, and reading labels
Cost becomes a major factor in the long run.
Specialty electrolyte products can cost a lot of money especially because you may be using several servings a day for months or years. This process involves passing a generation of patients whose treatments include building a layer by layer approach:
Taking regular table salt and food which make the foundation (1,4).
Adding one or two servings of a favourite product higher in sodium during times of increased demand (e.g. before exercise, or on hot days. (4)
Employing mixed DIY application with measured ways to burn cost while achieving certain sodium and potassium targets. (4,8)
Whatever the format you settle upon label literacy is an absolute.
Check:
- Sodium per serving.
- Serving size.
- Total number of servings per container.
- Projected monthly Cost based on what you eat.
Two products may contain similar looking compensatory amounts of sodium on the shelf, yet offer very different amounts of sodium per serving (1,4). The marketing language does not usually tell the whole storey.
In the end, the “best” electrolyte format is the one that has you getting sodium you need, that is fit to your physiology, and on the whole financially and practically sustainable.
Hypermobility, EDS, and POTS: special considerations
If you exist at the intersection of POTS and hypermobility, then you know already things aren’t usually simple. Salt advice that is viable for one person can be felt as totally different with hEDS or suspected MCAS. The physiology overlaps. The symptoms overlap and and sometimes they play an amplifying role upon each other.
The triad of POTS, hypermobile EDS, and MCAS
POTS, hypermobility EDS and mast cell activation syndrome are often said to co exist and this overlap is becoming recognised in specialist clinics (2,19). The concept here is not that they would be the same, but that the altered connective tissues, vascular dysfunctions and mast cell mediated inflammation may somehow interact to make orthostatic intolerance worse (2,19).
For some people, that results in more dramatic blood pooling. For others, it means unpredictable explosions played out with stress, infection, food, or hormonal changes. When these systems interact with each other, salt is still relevant but it enters a larger strategy as opposed to the sole solution.
How connective tissue laxity affects circulation and fluid needs
In hypermobility spectrum disorders and EDS, the collagen and other components of the connective tissue are altered (2). That can have an impact on the elasticity of blood vessels and valves in the veins. Lax veins are more likely to become distended when you stand since there is more pooling of blood in the legs and the abdomen (2, 19).
If more blood remains in the lower body then less blood returns to the heart. That causes decrease in the effective central blood volume and can aggravate orthostatic symptoms.(2,19). This mechanical pooling therefore goes some way to explaining the high prevalence of POTS in hypermobile cohort and hEDS.
Because of this some hypermocility patients are also more sensitive to the volume change. They may benefit from a combination of increased salt and fluid, compression garments and structured physical conditioning to improve the functioning of muscle pumps around lax joints.(2,16)
But this is important. High salt alone cannot correct laxity of the connective tissue. It can support volume but nothing structurally properties of veins can change. Expectations have to be realistic (2,4).
GI issues, histamine, and electrolyte strategies
Gastrointestinal symptoms are very common in POTS and hypermobility. Bloating, constipation, diarrhoea, nausea, early satiety and suspected MCAS are commonly experienced (2,19). These symptoms create problems with salt strategies in two ways.
First, diarrhoea and vomiting directly increase the fluid and electrolyte losses (2,8). Second, gastroparesis or early satiety reduces intake, thus it is more difficult to get enough salt and fluid to maintain volume.
PoTS UK state that MCAS like symptoms are becoming recognised in POTS and that foods, which are high in histamines, and some food additives can cause flares (1,2). Histamine contents in food may be amplified during storage and ripening (19). There are patients that find reducing high histamine foods or mast cell liberating foods (egg white, citrus, chocolate, crustaceans) raises their symptoms stability (19). Fresh, minimally processed foods are usually a better tolerance and refrigeration is important (19).
That said, histamine restricted diets can be very restrictive and may result in a decrease in quality of life. If a structured trial is not helpful in improving symptoms, the return to a balanced diet is reasonable (19). Restriction should be for a purpose and for a short period of time, not forever.
Screening for coeliac disease also applies. Coeliac disease seems to occur more in the POTS cohorts than the general population (2). If significant GI symptoms are present testing with tissue transglutaminase and endomysial antibodies should be done prior to removal of gluten, as testing requires ongoing gluten intake in order to be accurate (2).
For those patients who have significant sensitivity with GI symptoms or who have suspected MCAS, electrolyte products containing minimal flavourings, colours and additives may be easier to tolerate (2,4). Smaller and more frequent sips of dilute electrolyte solutions can sometimes work better than large, concentrated doses (2,4). When functional gut disorders such as IBS do coexist, structured diets of elimination or FODMAP type may be adopted by dietitians while salt, fluid and micronutrient intake must be regulated (2,4). Highly restrictive diets are recommended to be supervised and time limited (2,19).
Urological and gynaecological considerations
Bladder pain syndrome, interstitial cystitis, recurrent urinary tract infections, pelvic floor dysfunction and vulvodynia are found at increased rates in POTS plus hEDS cohorts (19,20). Mast cell activation has been theorised as one of the possible contributors (19,20). Dehydration may exacerbate many of these symptoms and optimising fluid and salt intake may aid in conjunction with specific targeted therapies (19,20).
Menstrual disturbances are also very common, with the period being heavy, painful and irregular (20). Mast cell activation and the release of heparin may be one of the factors responsible for heavier bleeding in some cases (20). Volume status may vary during the menstrual cycle which subsequently may change the severity of POTS symptoms (17). Some patients report worsening premenstrual and they help stabilise the symptoms by temporarily increasing salt and fluids during that period (17).
Joint pain, deconditioning, exercise, and volume status
Joint instability and pain often restrict activity in hypermobility and reduced activity can result in increased cardiovascular deconditioning (2,16). Deconditioning itself plays a role in the problem of orthostatic intolerance and this creates a difficult cycle.
Exercise programmes for POTS typically start with recumbent or semi recumbent exercise e.g. rowing, recumbent cycling, swimming etc. and progress gradually towards moving to upright exercise (16). The joint protection is key with hypermobile patients.
Salt and electrolyte strategies support these programmes by sustaining blood volume throughout training and decreasing post exercise orthostatic symptoms (3,4,16). Electrolyte intake before and during exercise may be especially helpful to those who are increasing levels of exercise as pain improves (4,16).
Salt is not a static therapy. In the case of hypermobility, it works best as part of a combined approach that takes into consideration volume, vascular support, muscle conditioning, as well as identifying and dealing with symptom triggers.
Practical protocols: how to trial salt and electrolytes safely
Salt strategies work best when they are structured and monitored rather than improvised.
Building a personalised plan with your clinician
A cautious, step by step approach may include:
1. Clearing the diagnosis of posture orthostatic tachycardia syndrome and reviewing diseases such as high blood pressure, kidney disease, heart disease, pregnancy or diabetes (1,7).
2. Forward to baseline home readings of sitting and standing blood pressure and heart rate for at least a few days along with scores of symptoms (4,7).
3. Estimating existing Sodium Intake from food and Beverages (1,4).
4. Agreed on to an initial increase, such as 1,000 to 2,000 mg per day, using food and possibly one electrolyte serving, then revaluating the symptoms, blood pressure and heart rate after one to two weeks (4,7).
5.No adjustment upward or downward based on response, as needed with periodic laboratory monitoring as needed (7,14).
The goal is not maximum salt. It is the minimal effective dosage.
Monitoring: blood pressure, heart rate, symptom diaries
The benefit versus risk of home monitoring: Home monitoring helps balance the benefit and the safety.
- Obtaining blood pressure and heart rate sitting and after standing for three minutes, several days per week (4,7).
- Observing symptoms such as dizziness, fainting and chest pain, breathlessness, swelling and headaches (4,7).
- Note diet, fluid intake, exercise and menstrual phase as hormonal changes can have an effect on volume (4,17)
If there is chronically reaching high value of systolic blood pressure to hypertension levels, or if swelling or breathlessness are present or headaches here worsens, then maybe necessary to reduce sodium consumption and control their intake. (7, 10, 11)
Red flag symptoms and when to reduce or stop
Take urgent medical advice if:
- New or worsening chest pain, shortness of breath or severe headache develops (7).
- Blood pressure gets extremely high or low, accompanied by neurological symptoms (7,10).
- Swelling of the legs or face or sudden weight gain indicate the presence of fluid overload (7).
- Kidney function decreases or creatinine or potassium increases (14).
At that point, salt and electrolyte strategies should be taken a look at reassessed. Other non pharmacological or pharmacological options for POTS may have to be considered (1,4,7).
Salt may be a powerful weapon in POTS. But like any tool, it runs best when wielded carefully, with respect to the much wider system you are trying to support.
Complementary lifestyle strategies
Salt really makes a false of POTS. But it works best when it is within the context of a broader plan. If you’re relying on sodium solely and you’re not watching your fluids, compression, exercise, sleep and general nutrition then you’re leaving potential gains on the table.
Fluids, compression, exercise, and sleep
Fluid intake
Salt is only effective if there is sufficient fluid available to retain (1, 3, 16). For most adults with POTS at least 2 litres/day is typical, however this can even work up toward the limit of 3 litres (depending on body size + climate + coexisting conditions (1, 16).
Many patients find it helpful to use front loading fluids. Drinking about 1 litre during the first hour of waking time can blunt the peak in heart rate that happens in the morning that is so common with POTS (16). Mornings often represent the time of lowest volume so this early boost can noticeably make a difference.
There is also evidence that the rapid ingestion of approximately 480 to 500 ml of water within 5 minutes is able to decrease the standing heart rate temporarily, as well as improve orthostatic tolerance (16). This is used sometimes as a short term rescue strategy for symptom flares. It is not a cure. But it can buy you stability in the time.
Compression garments
Compression entails decreased venous pooling which is directly related to one of the underpinning mechanisms in POTS (1, 16). The evidence suggests that abdominal plus leg compression is better than leg compression alone in the orthostatic disorders.16 Adolescents in tilt testing studies exhibit less tachycardia and symptoms with the combination of abdominal and extremity compression (16)
Waist high compression tights or abdominal binders are typically recommended. A compression level around 20 to 30 mm of mercury or more often is utilized but it depends on fit and tolerability. If you are not comfortable in a garment it will not be worn all the time. And it is the consistency where the benefit is.
Exercise
Functioning of the autonomic system and vascular tone, as measured by structured exercise improve over time (1,16). Most of the programmes start with recumbent or semi recumbent cardio exercises such as rowing, recumbent cycling or swimming, along with resistance training (16). Upright exercise is brought about gradually.
For people that are hypermobile, joint protection strategies are essential (2,16). Salt and fluids support these programmes by maintaining the volume of blood during and after exercise so that post exertional symptoms flare is reduced (3,4,16). When trying to lose weight or maintain your health, you should try to support your volume because it will make your exercise more bearable. And when exercise becomes more tolerable, there is the long term autonomic stability.
Sleep and pacing
Poor sleep causes an increase in sympathetic activation. In POTS, that can have the effect of amplifying symptoms (1,16). Basic sleep hygiene, consistency of bed times, not over stimulating daily activity crashes.
Elevation of the head of the bed by approximately 10 to 15 cm can decrease nocturnal diuresis and help sustain a good level of blood volume in the morning (16). It is a small change, but to some people it smoothes out the beginning of the day.
Diet quality beyond salt
Post meal considerations
After eating, there is a great increase of blood flow to the digestive system. In POTS this postprandial change can increase the severity of orthostatic tolerance 16. Large meals containing carbohydrates are more likely to cause the symptoms to appear.
Smaller and more frequent meals and moderation of refined carbohydrate consumption can minimise blood pooling in the post meal state and flares of symptoms (16). Some patients suffer from post prandial hypotension especially after a large meal (16). Modifying the sizes and composition of meals can be as much of a difference as modifying salt.
Nutrient rich dietary patterns
When determined by a higher sodium intake, even higher sodium intake matters. Even on a higher sodium intake, overall diet quality matters.
A dietary pattern that is rich in whole foods, fruits, vegetables, whole grains, healthy fats and lean proteins contains potassium, magnesium, calcium, fibre and antioxidants that promote cardiovascular and autonomic health (5,10). These nutrients may help balance some of these sodium risks when consumed over a long period of time (10,11).
The goal is not high salt and ultra processed food. It is high salt in nutrient dense framework.
Managing coexisting conditions
Fatigue is not always to be looked at as just POTS.
Anaemia, iron deficiency, decreased ferritin, vitamin B12 or folate deficiency as well as vitamin D deficiency all contribute to the aggravation of fatigue and simulate symptoms of orthostatic hypotension. (1,2) PoTS UK enlists that examples of low ferritin are more frequent in POTS populations.(1) Identification and correction of these deficiencies can enhance resilience and use through very high amounts of salt may be reduced.
Similarly, the management of IBS, MCAS and migraine could decrease flares of symptoms that worsen orthostatic intolerance (2,19). In more complicated cases the best results are often obtained by a multidisciplinary approach, which includes cardiology, specialists in autonomic dysfunction, dietitians, physiotherapists and, if required, gastroenterology, rheumatology or immunology (2,16).
Salt helps. But it is best used in conjunction with support of the rest of the system.
Frequently asked questions
Is salt or electrolytes better for POTS?
For many people it is most important they reach adequate sodium intake, whether that is achieved through food or electrolyte drinks, where there is a therapeutic target total daily sodium intake (3,4). Balanced electrolyte solutions are very helpful in cases of diarrhoea, vomiting, excessive sweating or in cases where the person’s food intake is poor (4,8).
Which electrolytes are good for POTS?
Sodium is key because of its capacity to increase the volume of blood. Potassium, magnesium and calcium are beneficial for heart rhythm, vascular tone and cardiovascular health (3,5,6). A potassium rich food diet and supplementation if deemed necessary may be beneficial to balance the increased intake of sodium (5,6,10).
What kind of salt should I use for POTS?
Any food grade salt can be an effective sodium enhancer including iodised table salt, sea salt or rock salt as they are mainly sodium chloride (18). Differences in trace minerals are insignificant. Choice may be according to taste and cost and iodine requirements (18).
How much salt should a person with POTS have per day?
Many expert sources recommend approximately 3000 to 10,000 mg of sodium per day for adults with POTS under medical supervision, which will be equivalent to somewhere around 7.5 grams to 25 grams of salt (1,3,15). PoTS UK recommends 6-10 grams of salt to be added to the diet for many adults, but dosing needs to be individualised and monitored, especially for children, older people and people with hypertension, or kidney patients (1,7,10).
Key messages
Salt and electrolytes can have a potent effect in POTS, and particularly in patients with low blood volume, it is important to remember that they are part of a much wider approach, involving the use of fluids, compression, music, and control of coexisting conditions (1,3,4).
Dietary salt (sodium) regimens help increase plasma volume and mitigate orthostatic tachycardia in the short term, but there are longterm cardiovascular and renal risks, especially among higher risk persons (3,7,10,11).
Due to the overlap of POTS, hypermobility, EDS and MCAS, integration in management is needed that focuses on volume, connective tissue, dietary triggers and nutritional deficiencies (2,19).
Front loading of fluids, rapid boluses of water as rescue therapy and combination abdominal plus leg compression can be added to the standard salt advice (16).
Pregnancy with POTS, where well managed conservatively, with attention to fluids, salt where indicated, compression and an approach used by multidisciplinary specialist teams (17), has favourable outcome. Children and adolescents should start using nonpharmacological measures and be salt dosed individualised and monitored by paediatric specialists.(1,8,16).
With proper monitoring and shared decision making, many people with POTS, especially, POTS with hypermobility, can determine a personalised group of treatments with salt, electrolytes and lifestyle strategies that will make a difference in improvement within established limits of long term safety (1,2,3,4).
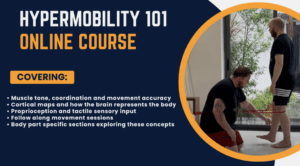
Enjoying Our Resources? Why Stop Here?
If you’ve found value in our posts, imagine what you’ll gain from a structured, science backed course designed just for you. Hypermobility 101is your ultimate starting point for building strength, stability, and confidence in your body.
References:
- PoTS UK (2023) Diet and fluids in PoTS. PoTS UK website information sheet, version V1.5, 25 March 2023. Available at: https://www.potsuk.org (Accessed: 16 February 2026).
- Tailor, V. and Khullar, V. (2023) ‘Urological and gynaecological considerations in PoTS’, in Postural Tachycardia Syndrome: A Clinician’s Guide to Diagnosis and Management. [Textbook chapter].
- Raj, S.R., Fedorowski, A., Sheldon, R.S. (2021) ‘Effect of high dietary sodium intake in patients with postural tachycardia syndrome’, Journal of the American College of Cardiology, 77(17), pp. 2174-2184. doi: 10.1016/j.jacc.2021.03.004.
- Williams, R., Black, B.K., Biaggioni, I., Shibao, C., Okamoto, L.E., Gamboa, A. (2022) ‘Salt supplementation in the management of orthostatic intolerance: Vasovagal syncope and postural orthostatic tachycardia syndrome’, Autonomic Neuroscience: Basic and Clinical, 237, 102842. doi: 10.1016/j.autneu.2021.102842.
- D’Elia, L., Brajovic, M., Klisic, A., Breda, J. (2025) ‘Effect of changes in potassium intake on blood pressure: a dose-response meta-analysis of randomized clinical trials’, Clinical Kidney Journal, 18(7), sfaf173. doi: 10.1093/ckj/sfaf173.
- Cook, N.R., Obarzanek, E., Cutler, J.A., Buring, J.E., Rexrode, K.M., Kumanyika, S.K., Appel, L.J., Whelton, P.K. (2009) ‘Joint effects of sodium and potassium intake on subsequent cardiovascular disease: the Trials of Hypertension Prevention follow-up study’, Archives of Internal Medicine, 169(1), pp. 32-40. doi: 10.1001/archinternmed.2008.523.
- de Beer, N.A., Anderegg, S., Im, J., Snoad, B., Parker, A. (2025) ‘Non-pharmacological treatment for postural orthostatic tachycardia syndrome’, JBI Evidence Synthesis, 23(1), pp. 4-83. doi: 10.11124/JBIES-23-00351.
- Li, H., Chen, X., Huang, H., Tang, C., Zhang, Q., Wang, C., Jin, H., Du, J. (2024) ‘Establishment and validation of a multivariate predictive model for the efficacy of oral rehydration salts in children with postural tachycardia syndrome’, Frontiers in Pediatrics, 12, 1092114. doi: 10.3389/fped.2024.1092114.
- Du, X., Jin, H., Wang, Y., Yan, H., Chen, X., Huang, H., Zhang, Q., Tang, C., Wang, C., Du, J. (2023) ‘Predicting therapeutic efficacy of oral rehydration salts in children with vasovagal syncope: development and assessment of a nomogram model’, Frontiers in Pediatrics, 11, 1164304. doi: 10.3389/fped.2023.1164304.
- Grillo, A., Salvi, L., Coruzzi, P., Salvi, P., Parati, G. (2019) ‘Sodium intake and hypertension’, Nutrients, 11(9), 1970. doi: 10.3390/nu11091970.
- Jaques, D.A., Wuerzner, G., Ponte, B. (2021) ‘Sodium intake as a cardiovascular risk factor: a narrative review’, Nutrients, 13(9), 3177. doi: 10.3390/nu13093177.
- Cirillo, M., Bilancio, G., Cavallo, P., Palladino, R., Zulli, M.V., Natale, F., Lombardi, C. (2021) ‘High sodium intake, glomerular hyperfiltration, and protein catabolism in patients with essential hypertension’, Cardiovascular Research, 117(5), pp. 1372-1381. doi: 10.1093/cvr/cvaa230.
- He, F.J., MacGregor, G.A. (2018) ‘Role of salt intake in prevention of cardiovascular disease: controversies and challenges’, Nature Reviews Cardiology, 15, pp. 371-377. doi: 10.1038/s41569-018-0004-1.
- Lv, J., Perkovic, V., Foote, C.V., Craig, M.E., Craig, J.C., Strippoli, G.F.M. (2023) ‘Altered dietary salt intake for preventing diabetic kidney disease and its progression’, Cochrane Database of Systematic Reviews, 1, CD010069. doi: 10.1002/14651858.CD010069.pub3.
- Cleveland Clinic (2024) POTS: Postural Orthostatic Tachycardia Syndrome – management recommendations. Cleveland Clinic patient information. Available at: https://my.clevelandclinic.org/health/diseases/16560-postural-orthostatic-tachycardia-syndrome-pots (Accessed: 16 February 2026).
- Eftekhari, H. and Bruce, D.L. (2021) ‘Non‑pharmacological management: hydration, diet and compression’, in Gall, N., Kavi, L. and Lobo, M.D. (eds) Postural Tachycardia Syndrome: A Concise and Practical Guide to Management and Associated Conditions. Cham: Springer Nature Switzerland AG, pp. 199–205.
- Borlase, D. and Nelson‑Piercy, C. (2021) ‘Pregnancy and postural tachycardia syndrome’, in Gall, N., Kavi, L. and Lobo, M.D. (eds) Postural Tachycardia Syndrome: A Concise and Practical Guide to Management and Associated Conditions. Cham: Springer Nature Switzerland AG, pp. 253–262.
- Sata, Y., Kistler, P.M., Iwai, S., Brandt, M.C., Tatschl, P., Krampf, L., Scherschel, K., Meyer, C., Sampath, S., Lennerz, C., Kuck, K.H., Veltmann, C., Goldberger, J.J., Gamboa, A. (2021) ‘High-sodium diet does not worsen endothelial function in female patients with postural tachycardia syndrome’, Autonomic Neuroscience: Basic and Clinical, 234, 102842. doi: 10.1016/j.autneu.2021.102842.
- Tailor, V. and Khullar, V. (2021) ‘Urological considerations in PoTS’, in Gall, N., Kavi, L. and Lobo, M.D. (eds) Postural Tachycardia Syndrome: A Concise and Practical Guide to Management and Associated Conditions. Cham: Springer Nature Switzerland AG, pp. 125–133.
- Tailor, V. and Khullar, V. (2021) ‘Gynaecological considerations in PoTS’, in Gall, N., Kavi, L. and Lobo, M.D. (eds) Postural Tachycardia Syndrome: A Concise and Practical Guide to Management and Associated Conditions. Cham: Springer Nature Switzerland AG, pp. 141–151.