- POTS and Exercise: The First Step Everyone Misses - 27 June 2025
- The Missing Link Between Breathlessness, Fatigue, and Chronic Pain: Understanding CO₂ Tolerance - 19 June 2025
- What is Mast Cell Activation Syndrome? - 12 May 2025
When it comes to Fibromyalgia and stretching, we are quite often told it will help. However, for those in pain, stretching can often be helpful for one, but a hindrance for another. In this blog, let’s explain why stretching can be beneficial when done correctly, but can also be detrimental when done incorrectly. As well as look at some of the different types of stretching for those with Fibromyalgia, and what is more likely to yield better results.
This article covers:
ToggleIs Stretching good for fibromyalgia?
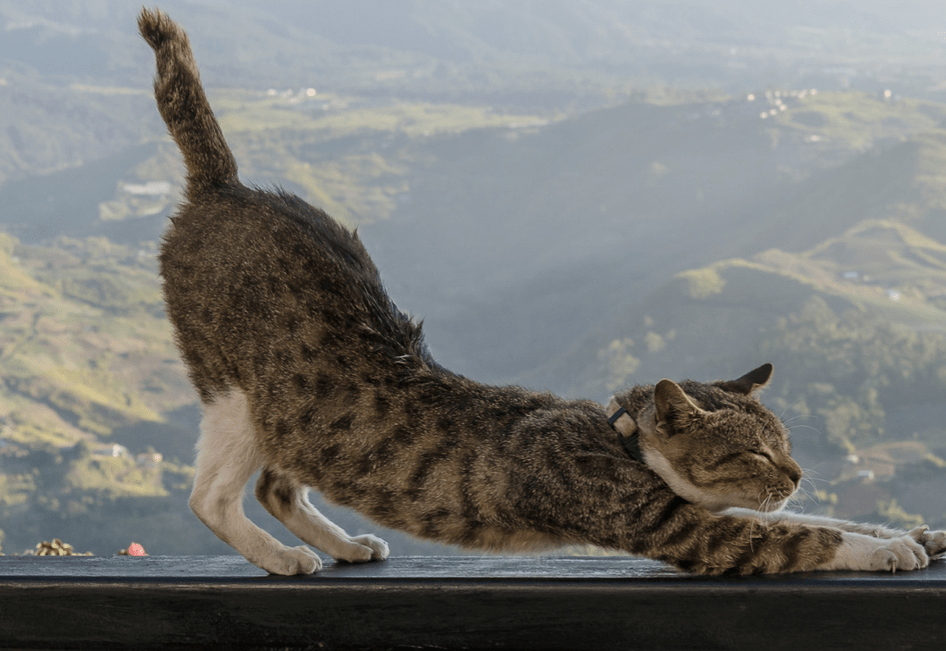
Everyone stretches. Athletes do it before training, my cat does it upon waking, and as I get older, I find myself doing it more and more. Generally though, for those with Fibromyalgia, they do it because it makes them feel better. When it comes to stretching this is a pretty good reason.
There is a lot of misinformation around stretching, most of which we first taught in school, and sadly, which is still taught. The evidence around stretching shows it doesn’t do half of what we have previously thought it had been doing. This is pretty worrying considering how mainstream it has now become!
We had thought for many years that the plastic deformation theory was king, wherein we thought muscles changed in length to account for increased muscle extensibility. However, as science challenges theories and conducts new research, things regularly get debunked and this is precisely what happened here: It was debunked!
Multiple studies showed that the previous evidence just did not support this particular theory. Stretching does not really change the length of tissue and, in the absence of disease, there are only three ways you can change a muscle’s length.
You can contract it, you can relax it, or you can go crazy on it with a scalpel, but I wouldn’t suggest the last one!
In fact, several muscles in your body are biomechanically impossible to stretch fully, seeing as your own body parts get in the way!
When you stretch your hamstrings, you will eventually hit a point where you can’t go any further due to discomfort and If you push a little deeper, you may perhaps even find it painful.
However, if you relax for a few seconds, breathe a little, take a big breath in followed by a big breath out, and slowly go deeper into the stretch, your brain can effectively turn down the discomfort and allow you further into the stretch, or at least allow more of what is commonly referred to “range of motion” (ROM). So, stretching is a lot more about the sensory stuff than actually muscle tissue, and at least the current evidence supports this theory.
So for those with chronic pain conditions such as Fibromyalgia, this can come as some relief. As pain often has a habit of convincing us that a particularly painful body part has something wrong with it. However, for those with a diagnosis of Fibromyalgia, they will have likely had various blood and imaging tests conducted showing that at least on a muscular-skeletal level, the tissue is ok. This means that reframing the narrative around stretching, to promote more of a sensory tinkering outlook, rather than a muscular one, allows people to feel more confident that they are not going to injure themselves when they do decide to stretch. Which in turn, is most likely going to relax you and make you less stiff in the first place.
Ultimately though when we do stretch, we are not making the tissue longer, we are only changing what we feel, and how comfortable our brains are with how much range of range of motion they are willing to put up with. It is this which allows us to get further into the stretch. When it comes to stretching with Fibromyalgia, this is an important thing to note. Being that stretching can provide an awful lot of rich and novel sensory information, with the propensity to override and change how you feel for the better. Not too shabby if I say so myself.
Why do people stretch?
Many people engage in various stretching routines every single day, and this is not just limited to those with Fibromyalgia. But, why do they stretch? And more importantly, is stretching doing what they believe it to be doing in the first place? Most of the evidence says probably not.
Stretching to warm up and prevents Injury:
It’s not uncommon to find droves of people stretching before exercise or even before something like running, with the assumption that stretching will warm them up and help their performance. Make them stronger or faster. However, you can not warm your muscles up, at least not metabolically anyway. If you use “warming up” in the sense of waking up your nervous system by say walking slowly, then a little faster, and then into a run, thus preparing it for actively, you could get away with using the term “warming up”
There is also the issue that the research around this area shows that stretching before exercise just doesn’t seem to do anything to help prevent injury. In fact, most of the research shows the complete opposite. Research shows that even just holding a stretch for a minute can lead to a small to moderate decrease in performance! There isn’t any solid data as to why this is the case, but with an educated guess you could surmise it may be something to do with impairing calcium release, a key component in muscle contraction.
To improve a joint’s range of motions:
This one may fairly surprising, as stretching does indeed help increase range of motion, but when comparing an increase in joint range of motion (flexibility) between both static stretching and weight training, generally we find that they both yielded around the same results. Yes, it’s like comparing cats to dogs in the research world, but definitely food for thought, when you consider the many benefits that come from swapping out stretching or weight training: Increased bone density, mood enchantment, strength, etc. Whilst flexibility has been a statement of health for hundreds of years, it really shouldn’t be. Studies show that how flexible a person is bears no real significance to mortality rate. Meaning that flexible people do not seem to live longer than their stiffer counterparts. Likewise, a person’s flexibility also does not correlate to fall risks or quality of life. Interesting then that flexibility has always been regarded as one of the core foundations of health. Institutions are slowly catching up to this idea though, most notably the Institute of Medicine’s 2012 report on measuring fitness in youth, which shows the lack of evidence linking flexibility tests with health outcomes, and does not recommend testing for flexibility in national youth fitness surveys.
Whilst flexibility has been a statement of health for hundreds of years, it really shouldn’t be. Studies show that how flexible a person is bears no real significance to mortality rate. Meaning that flexible people do not seem to live longer than their stiffer counterparts. Likewise, a person’s flexibility also does not correlate to fall risks or quality of life. Interesting then that flexibility has always been regarded as one of the core foundations of health. Institutions are slowly catching up to this idea though, most notably the Institute of Medicine’s 2012 report on measuring fitness in youth, which shows the lack of evidence linking flexibility tests with health outcomes, and does not recommend testing for flexibility in national youth fitness surveys.
Stretching to help with recovery:
Unfortunately, this myth is one that just does not seem to want to go away. The evidence strongly suggests that stretching does not speed up the healing process when it comes to post exercise soreness. We aren’t even sure what delayed muscle soreness is, let alone what helps it. So when it comes to using stretching for recovery, most studies show that it has no effect whatsoever, be that positive or negative. There is one caveat to this though, stretching could be seen as a good way to ensure that you do not lose range of motion after an injury. it isn’t going to speed up the healing process, but it can help restore lost range of motion.
Stretching with fibromyalgia just feels good:
I am 100% onboard for this being a reason for anyone with Fibromyalgia to stretch. It doesn’t depend on evidence to be true, as it’s totally subjective. If stretching makes you feel better, then stretch on my friends, your experience when it comes to anything, is yours alone, and no one can say it s not true. Stretching helps activate your parasympathetic nervous system, helping you to relax. It also helps release endorphins that make you feel good by helping to mask pain, and it gets you moving and increases blood flow, helping you to feel more awake and alert.
Stretching with Fibromyalgia
The general census when it comes to stretching is this; stretch the muscle and yank it beyond its length so it increases over time. But, given what we have discussed above, we know this ain’t the case. If you do have chronic pain and you suddenly start pushing your joints and tissues into positions that they are just not used to, then it’s probably going to lead to a fibromyalgia flare-up. There is an inherent danger in the unknown, this is hardwired into your very DNA. Your brain is no different. If you give it cause for concern, then it’s going to batten down the hatches and protect you by any means necessary. This can often mean pain. After all, how likely are you to repeat something that caused a huge flare up?
Fibromyalgia sufferers often feel stiff and tight. This is generally put down to muscles shortening over time with a lack of movement. Whilst there is some truth to this theory, most people assume that their range of motion is limited by literally short muscles, but this is very rarely the case. Even our incredibly flexible hypermobile clients feel stiff, yet they are incredibly flexible. There is a big difference between stiffness and inflexibility.
Your nervous system has a pre-determined length & strength for each of your muscles. This length & strength is based on many factors; previous injuries, current movement, and a healthy fear of moving, the list can be quite comprehensive based on the person.
Don’t believe me, then try this.
Whilst standing, take your right leg out to the side, up to 90 degrees, then put in back down on the floor.
Now do the same with your left leg.
Ok, you have a combined range of 180 degrees.
So, why can’t you do the splits?
Predetermined muscle length can change, have you ever noticed that your feel ridiculously stiff when you are ill?
Well, you can thank your immune system for that one. When you get an infection or the common cold, your body starts the inflammation process leaving you heavy, stiff, and weakened. Likewise, various lymph nodes can swell making areas such as your neck feel very stiff. So your preset length and tensions can change depending on the circumstances. Another example can be that of age or lack of movement (perhaps someone in pain). Age causes the cartilage that cushions your joints to dry out. And your joints make less of the synovial fluid that adds lubrication, causing you to feel stiffer.
Now imagine we have been told we have Fibromyalgia, we are in constant pain, and we fear moving as we don’t want to cause a flare-up. That is going to be something that factors into how stiff you feel. Those with Fibromyalgia can often be found exhibiting guarding and bracing postures due to pain, which is a surefire way to stiffen up.
With all of that in mind, does it make sense to grab a muscle and force it into a state of elongation?
Logic says not really. If our nervous system is not comfortable with changing the length or strength of a muscle it makes no sense to force it. Very much like appeasing an angry toddler, we have to work with it and persuade it that increasing the range of motion is a good thing. And when I say “It” I mean your brain.
We know stretching is more about the nervous system than the actual tissues, so think of stretching as a nervous system exercise, rather than a muscle one. When our body and brain are in a state of high alert due to pain, any sensory info coming from this type of traditional stretching can be deemed as dangerous for you.
OK, Matrix time….What if I told you there is a way to stretch whilst increasing muscle length, mobility and strength, all whilst calming our high-alert nervous system? Not possible? Alas, swallow the red pill and follow me down the rabbit hole.

Stretching for Fibromyalgia
In the video below I talk about Proprioceptive Neuromuscular Facilitation (PNF) stretching with an example of how to do it. But why does it work and how can you take advantage of it?
PNF allows the muscle to simultaneously contract whilst elongating. For your hyper-vigilant brain, this is very comforting. A muscle in a state of contraction is fairly safe (hence feeling stiff!) but at the same time, it is being elongated. Think of PNF as riding a bike with the stabilisers on. You are persuading your brain, in a safe and comforting way, that you can explore these new ranges of motion and it is safe. I call this the “move it to prove it principle.”
When our hyper-vigilant brain realises the new range of motion is safe, the resting state of the muscle begins to relax over time with consistency. More importantly, though, PNF stretching doesn’t require you to be super flexible in the first place. meaning you don’t need to stress your brain or tissues out to reap the benefits of PNF stretching. Likewise, if you have a muscle that can contract, you can PNF stretch it.
When the relaxation takes place is really where the magic happens. You are essentially given a window of opportunity to explore movement positively, to persuade your brain that this new range of motion is safe. Which when it comes to pain, is what it’s all about.
As an added Brucie Bonus, typically pain in the area will mellow for the same window of time. Imagine having an opportunity to move in a new way relatively pain-free for some time.
What would you do?
This is where folks on a programme will start to introduce new movements, and exercises and enjoy feeling “normal” for that window of time. Repeated over time, this window of time expands until the brain is persuaded that this is safe and it becomes the new baseline normal.
Although the premise of PNF seems simple, the science behind it is incredibly complex. A favourite saying of mine whilst in the studio is “It’s as simple & complex as that.”
Remember: The length and strength of every muscle in our body are dictated by our nervous system.
Tips for stretching with Fibromyalgia
- Stretching to very mild discomfort is just as beneficial as “Hard Core” stretching, so work smarter, not harder.
- Stretching is more about your nervous system and safety than the physical muscles, so keep this in mind.
- Slowly does it. As your progress with stretching, you can try and move a little more, push a little deeper, but start slow.
- Once you feel more comfortable with PNF stretching, you can move to static stretching, or even try Yoga!
- Stretching is a very rich sensory experience, so go slow and concentrate on what you are feeling.
- Motion is lotion for your joints, they are designed to move, but if your brain is hypervigilant when it comes to movements, reduce the load exposure. Split the amount of stretching you are doing into bite-size chunks throughout the day.
–The Fibro Guy Team —
P.s.
We hope you enjoyed reading. If it is something you are interested in, then we don’t mind filming a little gentle stretching routine. Just let us know in the comments!
Looking for more articles on Fibromyalgia?
Fibromyalgia and Osteoarthritis
Fibromyalgia and Costochondritis
Fibromyalgia headaches
Fibromyalgia and Sciatica